The stemless shoulder arthroplasty also known as resurfacing has gained popularity. When a new implant is introduced two basic questions need to be answered to identify its value:
a. What problem does the new implant solve? or "why is it superior to the existing implants?"
b. How "big" is that problem?
The theory in the development of stemless prostheses for shoulder replacement is the advantage of "bone preservation" and the ability for easier future revision. What we know today is that most shoulder arthroplasty constructs fail at
the glenoid (glenoid component loosening) and that the humeral stem is rarely the reason for revision. Thus, to answer the second question of how big the problem is, it is probably insignificant.
It terms of the first question it seems that a smooth standard stem which is press fitted or a small size stem prosthesis with porous coating is rarely a problem during revision shoulder arthroplasty when extraction is required. For that reason, the theory of bone preservation is not very convincing. The indication, in my opinion, of using a stemless implant is when there is an existing metaphyseal proximal humerus malunion and implantation of a stem is problematic due to
deformity of the humeral canal.
The problems that we see with the stemless shoulder implants are the following:
a. when the shoulder is painful it is nearly impossible to identify radiographically if the stemless implant is loose
b. In the Scandinavian and Australian registries they have higher revision rates compared to standard length hemiarthoplasties
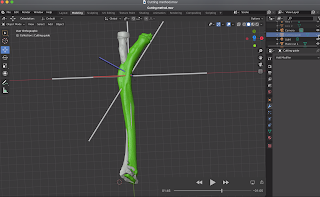
c. Most of these implants are malpositioned due to the difficulty in establishing the neck shaft angle. An intramedullary "rod" is not used and frequently there is varus positioning as in the case below.
This patient had pain for 5 years after a Copeland resurfacing hemiarthroplasty. Radiographic analysis as shown below illustrates two problems:
a. the neck shaft angle indicates 124 degrees of inclination when the normal is 130-140 degrees. When the average neck-shaft angle of the 2058 humeri was calculated, 77% of the humeri had an angle of between 130 degrees and 140 degrees. Although, the effect of a varus or valgus alignment of the prosthetic humeral head on the center of rotation of the articular surface seems small, it is unknown what the effect in the long term is.
b. There is 'overstuffing' of the shoulder joint which increases contact forces within the joint and tension to the rotator cuff leading to stiffness and pain which was the main reason that this patient was referred to us.
Neck shaft angle of 124 degrees
Center of rotation is medialized indicating overstuffing
axillary view indicates medialization of the humeral center of rotation
Revision to anatomic total shoulder arthroplasty with neck shaft angle of 134 degrees
Restoration of the center of rotation of the humerus
After the revision surgery to a total shoulder arthroplasty the patient had 160 degrees forward elevation, no pain and was pleased with the outcome at 6 months postoperatively.